Aged Care Reforms 2025: A Micro-Practical Leadership Playbook for Providers
Australia’s care system is entering a decisive phase of change and positive improvement. A new, rights-based Aged Care Act is scheduled to commence in November 2025, with the Support at Home program moving to the same start date. Simultaneously, ongoing requirements such as minimum care minutes and 24/7 registered nurse coverage will continue to reshape workforce planning, funding, and governance functions. For leaders of aged care, disability, and community providers, these changes are not just compliance updates. These mark strategic shifts that are likely to be sustained and which demand the development of new capabilities for your organisations and leaders across multiple areas including finance, risk, operations, and culture (Australian Government Department of Health, Disability and Ageing, 2025a).
This micro-guide distils what is changing, why it matters, and a step-by-step pathway to prepare your organisation. For those of you interested in our learning programs, each action is linked to the leadership capabilities developed in ICM’s Mini-MBA in Health Services Management.
1) What’s new and why it matters in 2025
A rights-based Aged Care Act (from 1 November 2025)
The new Act reframes obligations around the rights of older people, strengthening provider accountability, transparency, and quality expectations. Rights-based legislation typically heightens scrutiny of governance, incident response, and consumer engagement. Many services still rely on policies designed for a different regulatory era (Australian Government Department of Health, Disability and Ageing, 2025a).
Support at Home aligned to the same date
The government has confirmed that the start of Support at Home, replacing current in-home arrangements, will now align with the Act on 1 November 2025. The deferral gives providers extra time to redesign service models, pricing, and rostering. However, it also extends the period of uncertainty for clients and teams, which leaders must manage with clear communication (My Aged Care, 2025; Aged Care Online, 2025; Ozcare, 2025).
Care minutes and 24/7 RN are here to stay
Mandatory care minutes, including a registered nurse component, are now a bedrock of residential aged care operations and funding. Providers must plan rosters, recruitment, and skill mix to meet targets and report performance transparently (Australian Government Department of Health, Disability and Ageing, 2025b, 2025c, 2025d).
Funding and sustainability are still front-of-mind
Following the Aged Care Taskforce’s funding recommendations (2024), debate continues about how to balance affordability, quality, and sustainability. Modelling highlights cost pressures and the need for governance maturity and productivity improvements (MinterEllison, 2024; StewartBrown, 2024; Australian Government Department of Health, Disability and Ageing, 2025e).
Cross-sector signals from the NDIS Review
The NDIS Review Final Report (2023) continues to influence workforce, market stewardship, and compliance expectations across disability services. Its implementation roadmap emphasises quality, sustainability, and better integration across systems. These capabilities also apply directly to aged care leadership (NDIS Review Panel, 2023; Australian Government Department of Health, Disability and Ageing, 2025f).
2) The leadership implications: from compliance to capability
There’s an old saying that: reforms change rules, leaders change results. Across boardrooms and frontline teams, the 2025 landscape demands:
Governance that actually works in practice. Boards and executives will need clearer oversight of rights, risk, and quality, along with sharper responses when things go wrong.
Workforce strategy, not just rostering. Care minutes and RN coverage require sustainable pipelines, retention strategies, and skill-mix optimisation.
Financial acumen linked to outcomes. Budgets must reconcile workforce costs with quality requirements and funding rules.
Evidence-ready quality systems. Providers need to demonstrate consistently that care is safe, person-centred, and improving.
Stakeholder engagement with purpose. Consumers, families, unions, regulators, and partners expect transparency, respect, and rapid communication.
These are not simple ‘tick-box’ capabilities. They are integrated leadership skills - the kind of skills our Mini-MBA builds through case-based learning, simulations, and a workplace impact project.
3) A practical, 90-day plan to get ready
Day 0–30: Get the facts straight
Map the reforms to your services: Identify which parts of your portfolio are affected by the Act start date, Support at Home alignment, and care minutes.
Brief the organisation’s board: Present a concise rights-based risk and gap analysis with clear priorities, timelines, and residual risks.
Check your data and dashboards: Ensure you can track care minutes, RN coverage, incidents, complaints, and corrective actions weekly, not just quarterly.
Update consumer communications: Prepare plain-English FAQs for clients and families about what will and will not change on 1 November.
Day 31–60: Close the biggest gaps
Roster to reality: Rework rosters and recruitment plans to hit care-minute targets sustainably.
Tighten governance: Clarify decision rights, escalation pathways, and board reporting packs to make rights-based oversight tangible.
Rehearse regulatory responses: Run a tabletop exercise: incident → investigation → apology → improvements → board notification.
Refactor policies: Replace legacy policy language with rights-based framing (dignity, choice, cultural safety) and identify where training is required.
Day 61–90: Prove outcomes, not effort
Quality ‘mini-audit’: Test your evidence trail against sta4) Five high-value projects to launch now
Rights-based care design sprint (2–3 weeks). Co-design a core set of care principles and scripts with staff and consumers, then convert them into quick-reference job aids.
Workforce stability pack. Define a retention bundle: predictable rosters, micro-credential pathways, mentoring, and wellbeing supports linked to care minutes.
Board assurance bundle. Introduce a monthly dashboard covering rights incidents, complaints cycle-time, care minutes compliance, corrective actions, and consumer sentiment.
Support at Home pricing and pathway redesign. Map intake → assessment → service plan → feedback loop. Ensure pricing and communications are transparent before go-live.
Regulatory response playbook. Pre-author templates for notifications, apology letters, Corrective Action Plans, and public statements.ndards and fix documentation gaps.
Consumer voice: Start a short pulse survey and publish “you said / we did” updates.
Financial guardrails: Stress-test budgets under different workforce scenarios and funding assumptions.
Publish a reform roadmap: Share a one-pager with staff and clients that outlines what happens by November, who is responsible, and how questions are answered.
4) Five high-value projects to launch now
Rights-based care design sprint (2–3 weeks). Co-design a core set of care principles and scripts with staff and consumers, then convert them into quick-reference job aids.
Workforce stability pack. Define a retention bundle: predictable rosters, micro-credential pathways, mentoring, and wellbeing supports linked to care minutes.
Board assurance bundle. Introduce a monthly dashboard covering rights incidents, complaints cycle-time, care minutes compliance, corrective actions, and consumer sentiment.
Support at Home pricing and pathway redesign. Map intake → assessment → service plan → feedback loop. Ensure pricing and communications are transparent before go-live.
Regulatory response playbook. Pre-author templates for notifications, apology letters, Corrective Action Plans, and public statements.
5) The capability gap (and how to close it)
Most provider teams report two kinds of capability gaps:
Horizontal gaps across functions such as finance not talking to clinical governance or HR not being tied to quality targets.
Vertical gaps from board to frontline such as strong values but unclear escalation and decision rights.
Closing these gaps requires your leadership team to develop an integrated skillset. That is why our Mini-MBA combines strategy, finance, governance, quality, risk, workforce, innovation, and stakeholder engagement into a coherent learning journey. Leaders can then connect decisions across the organisation.
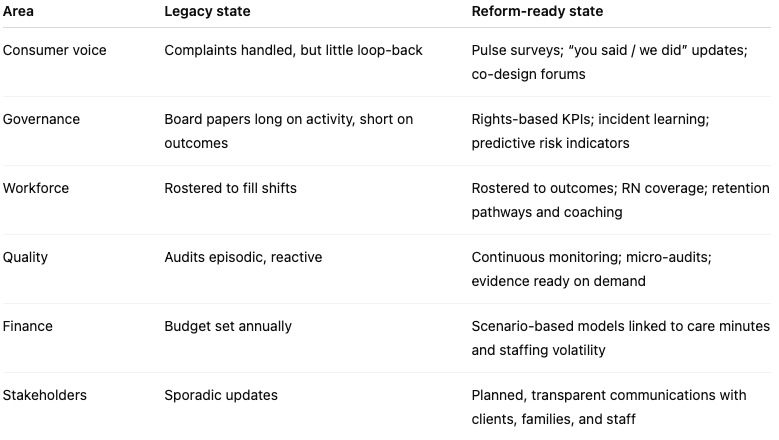
6) What great looks like under the new Act
7) How the ICM Mini-MBA supports reform readiness
Case-driven learning. Every module uses realistic scenarios from aged care, disability, and mental health services so you learn in the same complexity you work in.
Programmatic approach. Short tasks build into a capstone transformation plan you can implement, often in the same quarter.
Specialisations that matter. Choose pathways like Aged Care Leadership & Governance, Quality & Risk, Workforce Leadership, or NDIS Business & Compliance. The specialisation shapes your assessments and your workplace project.
Direct workplace impact. Expect to leave with a reform-ready governance brief, a workforce plan aligned to care minutes, and a quality system that is audit-ready.
Conclusion
The 2025 aged care reforms present both disruption and opportunity. Providers that treat them purely as compliance exercises risk falling behind. Those that approach them as a catalyst for strategic capability-building will be positioned to lead. The ICM Mini-MBA in Health Services Management equips leaders with the integrated skills to not only meet the new legislative and operational requirements but also to thrive in a more transparent, accountable, and consumer-focused care environment. By combining rights-based governance, financial acumen, and workforce strategy with real-world case learning, this program bridges the gap between reform readiness and long-term organisational resilience.
References
Aged Care Online. (2025). Support at Home reform updates. Aged Care Online.
Australian Government Department of Health, Disability and Ageing. (2025a). New Aged Care Act overview. Canberra: Commonwealth of Australia.
Australian Government Department of Health, Disability and Ageing. (2025b). Mandatory care minutes: Guidelines. Canberra: Commonwealth of Australia.
Australian Government Department of Health, Disability and Ageing. (2025c). RN coverage requirements. Canberra: Commonwealth of Australia.
Australian Government Department of Health, Disability and Ageing. (2025d). Care minutes compliance reporting. Canberra: Commonwealth of Australia.
Australian Government Department of Health, Disability and Ageing. (2025e). Funding sustainability in aged care. Canberra: Commonwealth of Australia.
Australian Government Department of Health, Disability and Ageing. (2025f). NDIS Review implications for aged care. Canberra: Commonwealth of Australia.
MinterEllison. (2024). Aged care funding reform insights. MinterEllison Consulting.
My Aged Care. (2025). Support at Home start date announcement. Australian Government.
NDIS Review Panel. (2023). NDIS Review final report. Canberra: Commonwealth of Australia.
Ozcare. (2025). Preparing for Support at Home. Ozcare.
StewartBrown. (2024). Aged care financial performance survey. StewartBrown Advisory.